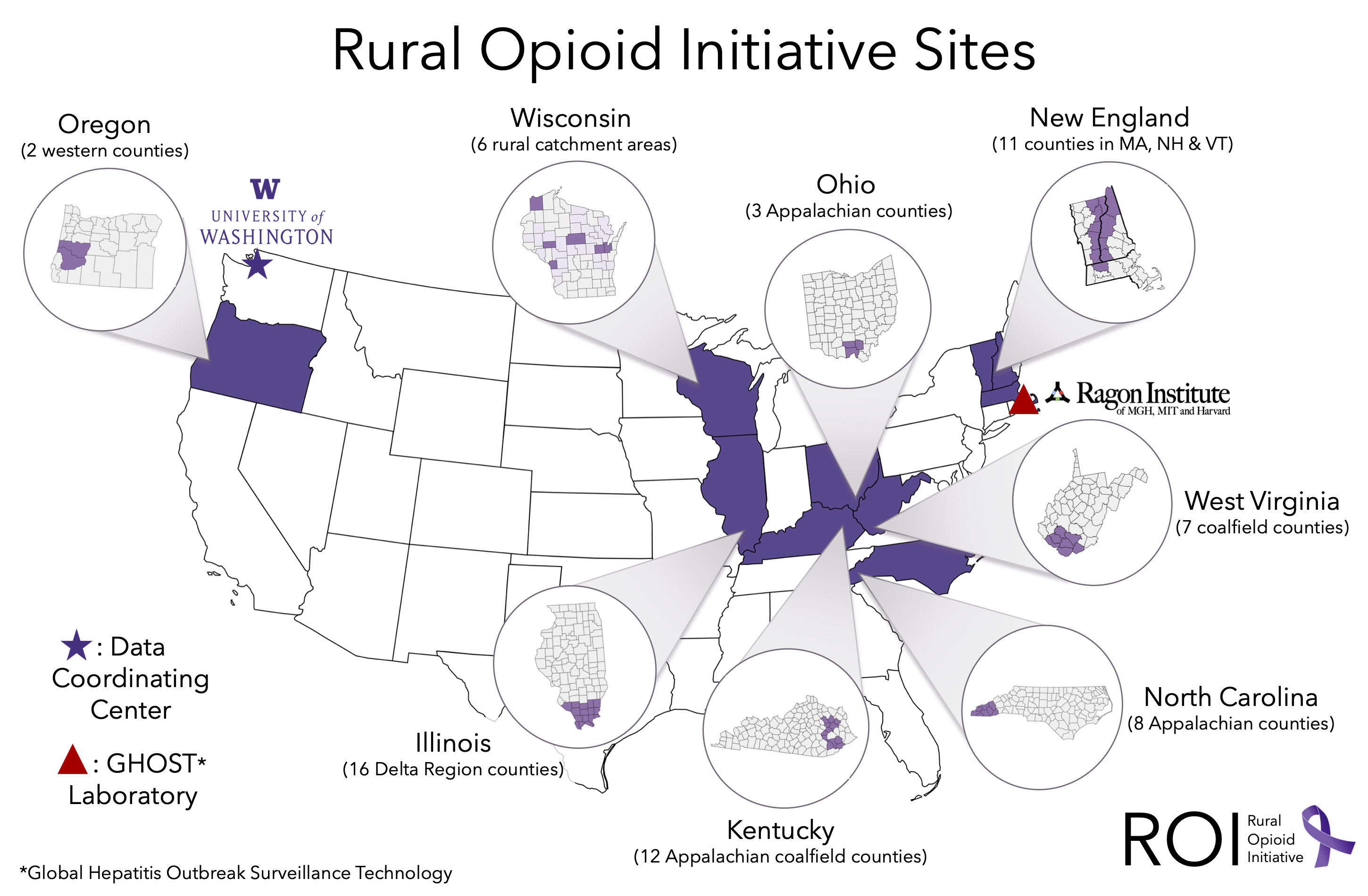
ROI Research Consortium Studies
Illinois
Kentucky
North Carolina
New England
Ohio
Oregon
Wisconsin
West Virginia
GHOST Laboratory
Data Coordinating Center
Illinois
Ending transmission of HIV, HCV, and STDs and overdose in rural communities of people who inject drugs (ETHIC)
Improving the health outcomes of individuals with opioid addiction and injection drug use requires a broad understanding of the structural, sociocultural, network, and individual level factors impacting high risk injection practices and access to care and services. ETHIC employs a mixed analytical approach including predictive modeling, GIS analysis, qualitative and survey analysis, network methods, and infectious disease epidemiology to inform the implementation of expanded harm reduction services and access to clinical services for people who inject drugs in rural areas of southern Illinois.
PIs: Mai Pho, MD, MPH & Wiley Jenkins, PhD, MPH
More Information Study Overview Study Outcomes

Kentucky
Kentucky Communities and Researchers Engaging to Halt the Opioid Epidemic (CARE2HOPE)
CARE2HOPE employs community/academic partnerships to build effective, evidence-based, community-grounded public health responses to combat the intertwined epidemics of heroin and non-medical prescription opioid injecting, overdoses, and HCV, and imminent HIV outbreaks, in 12 of the hardest hit rural counties in the US. Located in Central Appalachian Kentucky, 10 of the 12 counties are in the top 5% for HIV/HCV vulnerability in the US. Most counties are in coal country, a priority area.
PIs: April Young, PhD & Hannah Cooper, ScD
More Information Study Overview
North Carolina
Mitigating the Outcomes Associated with the Injection Drug Use Epidemic in Southern Appalachia (SA-TLC)
The objective of SA-TLC is to train health care providers to provide hepatitis C virus care and other services to people who inject opioids. It will also employ bridge counselors to link people who use opioids to services across different settings (e.g., local health departments, substance use disorder treatment programs) and establish syringe service programs in rural western North Carolina. If these activities are effective, they could be scaled up in rural areas across the state and reduce opioid-related morbidity and mortality.
PI: William Zule, DrPH
Study Overview
New England
Drug Injection Surveillance and Care Enhancement for Rural Northern New England (DISCERNNE)
HIV, HCV, overdose, and sexually transmitted infections are important, treatable causes of morbidity and/or mortality for persons who inject drugs (PWID) in rural areas, where access to specialty care and services is limited. This two-stage, mixed-methods study will examine epidemiology, infectious consequences, and service accessibility among young PWID in rural counties in Massachusetts, New Hampshire, and Vermont, and then implement an integrated telemedicine approach to treat OUD and reduce HIV, other infectious complications and overdose. It will inform efforts to improve access to services for PWID and reduce the toll of the opioid crisis in rural areas of the United States.
PIs: Peter Friedmann, MD, MPH & Thomas Stopka, PhD, MHS

Ohio
Implementing a Community-Based Response to the Opioid Epidemic in Rural Ohio
Rural America is confronting an opioid epidemic. The objective of this study is to assess if a service delivery plan can reduce barriers to key drug-related services in order to improve opioid-related outcomes including overdose, infectious diseases, and treatment. If successful, the study will set up a toolbox for local health departments that allows them to assess their opioid epidemic rapidly and adapt the service delivery plan to implement locally.
PIs: William Miller, MD, PhD & Vivian Go, PhD


Oregon
Oregon HIV/Hepatitis and Opioid Prevention and Engagement (OR-HOPE) Study
The U.S. Department of Health & Human Services identifies opioid use disorder (OUD) as a national crisis, and the consequences are particularly adverse in rural America. OUD treatment can decrease HIV and Hepatitis C (HCV) transmission, but access to evidence-based services is often limited in rural US due to barriers such as limited provider expertise and limited access to testing and treatment services for HIV, HCV, and OUD. In OR-HOPE community-based peer care coordinators engage people with OUD to assess HIV/HCV risk, conduct rapid HIV and HCV testing, and link them to treatment services.
PI: Todd Korthuis, MD, MPH

Wisconsin
Community-based, client-centered prevention homes to address the rural opioid epidemic
Rural-dwelling people who inject heroin and other opioids are a highly marginalized population. Poor access to medical and prevention services leaves residents of many rural U.S. communities vulnerable to preventable harms of injection opioid abuse. The overall objective of this project is to implement an innovative yet widely replicable service delivery model which we have named the Community-Based, Client-Centered Prevention Home. The project will use mixed-methods to conduct a comprehensive needs assessment in 6 rural counties across Northern Wisconsin. Using an implementation science framework, we will develop and evaluate a service coordination model within an existing network of rural syringe service programs. Innovative features of this approach include use of a mobile health application to enhance the reach of prevention case managers, who will facilitate clients' access to a comprehensive package of 9 evidence-based prevention services.
PIs: Ryan Westergaard, MD, PhD, MPH & David Seal, PhD
More Information

West Virginia
Rural West Virginia Responds to Opioid Injection Epidemics: From Data to Action
The southern West Virginia coalfields are the epicenter of the injection opioid epidemic ravaging central Appalachia and other rural areas in the U.S., where the consequences— rates of hepatitis B and C and overdose deaths—are the highest in the nation. This area is also at high risk of an HIV outbreak similar to the one in rural southeast Indiana in 2014-15. The objectives of this project are to improve HIV testing and case-finding, develop harm reduction programs, and create an integrated model of testing and linkage to care to prevent an HIV outbreak in the 8 hardest-hit southern coalfield counties.
PIs: Judith Feinberg, MD & Gordon Smith, MD, MPH

GHOST Laboratory
Next-Generation Sequencing Center for GHOSTing Hepatitis C Virus: Transforming Community Based Molecular Surveillance and Outbreak Investigation
To effectively intervene in the growing incidence of new HCV infections in persons who inject drugs (PWID), and prevent HCV and HIV epidemics, such as the one in 2015 in Scott County, Indiana, laboratory support for ROI consortium study sites is needed to generate rapid and robust viral sequence data to enhance the investigation of HCV outbreaks and transmission networks among PWID, including those with concurrent HIV infection, and to help guide public health interventions to disrupt HCV transmission in PWID communities.
PI: Todd Allen, MD, PhD

Data Coordinating Center
Rural Comorbidity and HIV consequences of Opioid use Research and Treatment Initiative Data Coordinating Center (DCC)
Narrative studies are key to understand the evolving and increasingly rural opioid epidemic in the United States. Individual studies address key questions regarding opioid use and its consequences in the United States but cannot address many of the important questions related to HIV risk and other consequences which require larger sample sizes and greater generalizability. By integrating and linking data across ROI consortium studies, we will achieve the sample sizes needed to better understand the consequences, impacts, and other lessons that can be learned regarding opioid use in rural communities.
PIs: Heidi Crane, MD, MPH & Judith Tsui, MD, MPH
